The Science of Depression: Causes, Symptoms, and the Role of Neurotransmitters

When I was younger, I was confused about the role of neurotransmitter in depression. How certain hormones could interface with the most complex organ in the body: how they alter our brain to change how we feel, eat, and sleep?
What is much more interesting is that depression has become much more prevalent today than ever.
In fact, in 2023, the Centers for Disease Control Report addressed suicide, which is usually a complication of depression, as the second leading cause of death in the United States in 2021.
It’s overwhelming how could a change in the role of neurotransmitter in our bodies can lead to depression, which is a feeling of hopelessness, low mood, and prolonged sadness.
What is even more intriguing is that people often underestimate the role of neurotransmitter in depression and the impact of depression.
simply because they don’t understand how these chemicals function and how antidepressants medications can be effective.
In this blog, we are going to explore what is depression, its causes, and the role of neurotransmitter in depression.
Understanding Depression: An Overview
Depression, or major depressive disorder, is a common and serious mental health issue. This concept may sound vague to you, but you can think of depression as a long period of sadness with other symptoms, such as a loss of interest, which makes it a barrier for you to work and live properly.
The Centers for Disease Control and Prevention (CDC) reported that 21 out of 100 U.S.-based adults experienced symptoms of depression in 2024. This rate means that depression is a common issue among adults.
Interestingly, symptoms of depression vary from person to person, and this could be a result of many factors like genetics, lifestyle, resilience, and chemical contributions.
The American Psychiatric Association created a diagnostic creator for depression named DSM-5, which includes the following symptoms:
Psychological symptoms:
- Feeling sad, empty, and low mood.
- Losing interest or pleasure.
- Feeling hopelessness or helplessness
- Feeling worthlessness or guilt
- Difficulty concentrating, remembering, or making a decision.
- Thoughts of death or suicide.
Physical symptoms:
- Changes in sleep( too much or too little)
- Changes in appetite(eating too much or too little)
- Low energy and fatigue
- Unexplained physical aches and pains such as headaches or stomach issues.
Please note that at least five of these symptoms must be present daily, and one of them must be either a depressed mood or a loss of interest or pleasure.
What causes depression?
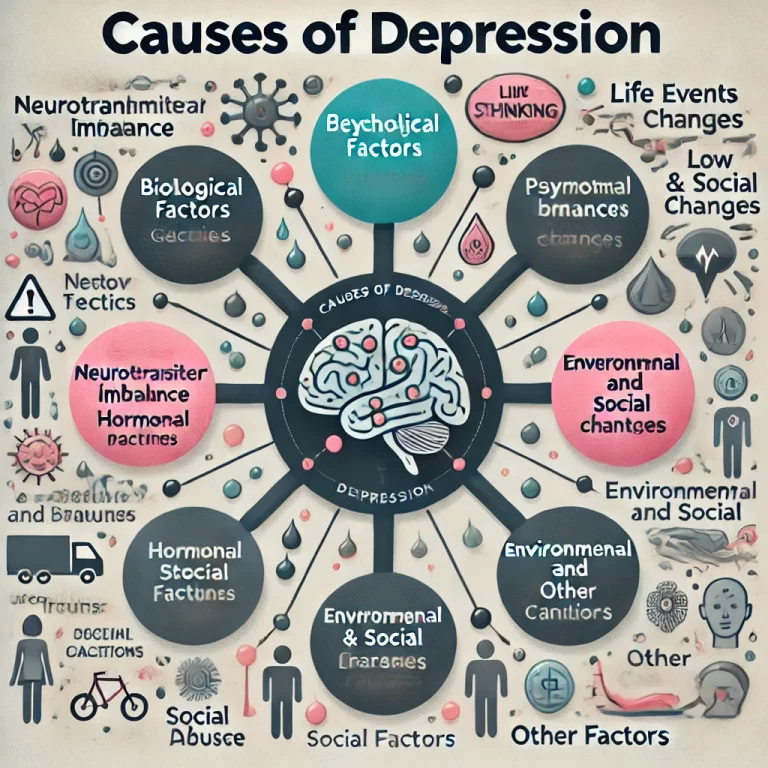
I once believed that genetics was the sole cause of depression, but I learned that depression is a multifactorial disorder. This means that various factors can contribute to its development. Additionally, some of these factors may support or exacerbate the onset of depression.
We can classify the causes into four main categories:
A. Biological cause:
- Family history: family history, especially among first-degree relatives, significantly increases the likelihood of depression compared to other factors.
- Neurotransmitter imbalance: These chemical messengers play a significant role in regulating our moods, feelings, sleep, and appetite. An imbalance in these neurotransmitters could result in depression. The cause of this imbalance is not specifically any condition that results in imbalance.
- Hormonal changes: Hormones usually influence each other’s levels and functions, which can be explicitly seen during the menstrual period, where women often experience depression, in addition to depression associated with pregnancy and menopause.
- Brain Structure and Function: Any changes in brain structure and function could result in unfamiliar side effects. For example, changes in specific parts of the brain, such as altered activity in the prefrontal cortex and amygdala, are associated with depression.
B. Psychological Factors:
- Negative thinking: Interestingly, research has found that negative thinking could alter your mood in the long run. It shows that a prolonged period of negative thinking could demotivate you and result in a depressive mood and symptoms.
- Low self-esteem: Negative thinking and low self-esteem usually occur together, and their main effects result in chronic stress, demotivation, loss of interest, and sleep and eating issues; all of these contribute to the development of depression.
- Stress and Trauma: Stress and trauma are among the most common causes of depression, anxiety, and other mental illnesses. Exposure to prolonged stress or traumatic events alters neurotransmitters, which results in the development of depression.
C. Environmental and Social Factors:
- Life Events and Stressors: Life events resulting in stress and prolonged sadness are common causes. Things like the loss of a loved one or stress related to war, financial issues, or chronic illness can significantly predispose individuals to depression and anxiety.
- Social Isolation and Lack of Support: We are supposed to be together because we need each other, and interestingly, research shows that social isolation and lack of support could predispose us to depression.
- Childhood Adversity: The American Journal of Preventive Medicine has found that childhood experiences such as abuse and neglect are linked to a higher risk of depression and other health problems in adulthood.
D. Other Factors:
- Substance Abuse: Drugs, alcohol, and smoking that interfere with normal brain function significantly lead to abnormal brain function res, result in mental illness, and trigger and exacerbate depressive symptoms.
- Medical Conditions: Medical conditions, specifically chronic illnesses such as diabetes and heart disease, are usually associated with the development of depression and anxiety due to uncertainty and sadness, which result in a depressive mood.
Whatever the cause, the main effects are changes in key role neurotransmitters, alterations in brain function, prolonged stress, and disruption of the reward system.
However, understanding the exact cause of depression is a crucial step for effective treatment and lifestyle changes that eliminate triggers and root causes.
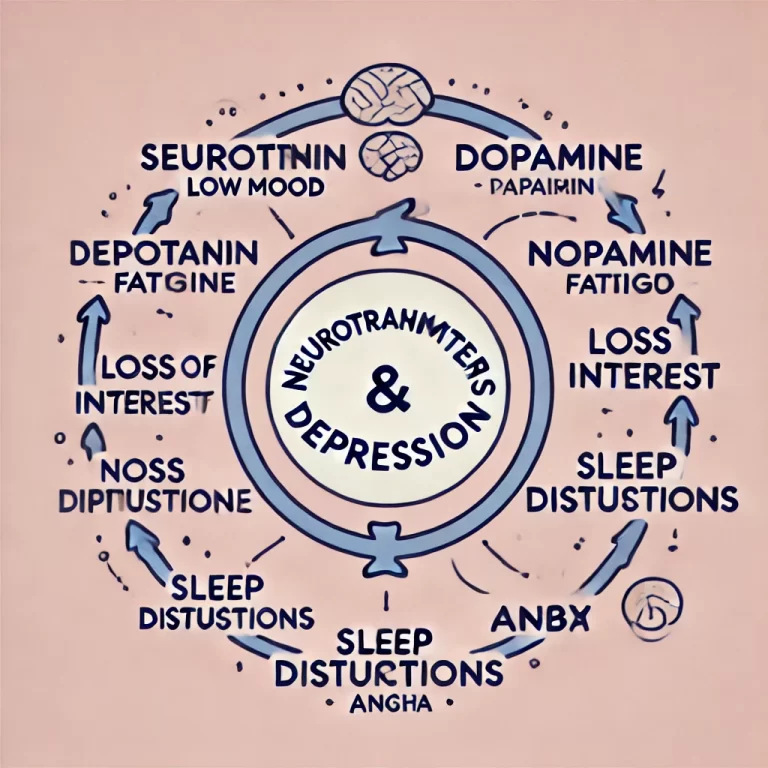
Neurotransmitters Associated With Depression
Certain neurotransmitters play a significant role in moods and feelings. What are they? Neurotransmitters are chemical messengers in neurons (the brain’s nerve cells) that regulate moods and emotions. They also influence motivation, appetite, and sleep.
Serotonin:
The body releases this feel-good hormone from different parts, most commonly from the stomach. It regulates our mood, sleep, and appetite—an imbalance in serotonin results in a low mood, which could progress to depression and sleep issues.
Dopamine:
This neurotransmitter is known to have a rewarding role in pleasure, motivation, focus, and decision-making. If dopamine levels decrease, you may lack motivation, feel fatigued, and have a low mood.
Norepinephrine (Noradrenaline):
The body releases this hormone in the fight-or-flight condition. For example, when someone frightens you, your brain and body release norepinephrine, which increases alertness, attention, and energy. Therefore, a decrease could result in low energy and difficulty concentrating.
GABA (Gamma-aminobutyric acid):
This works differently, stopping certain neurotransmitters to promote relaxation and calmness. For example, when the GABA level is low, anxiety and overthinking result in increased brain activity.
These neurotransmitters and hormones regulate communication between nerve cells in the brain. They are supposed to be in balance to manage emotional well-being and other functions.
In depression, the levels of these neurotransmitters, specifically serotonin, affect how the brain’s nerves communicate, resulting in abnormal function regarding feelings, appetite, and sleep, alongside other issues.
Interestingly, researchers found that one neurotransmitter’s balance can alter the levels of other neurotransmitters.
For example, serotonin influences dopamine, glutamate, and GABA release. This explains why fatigue, loss of interest, and motivation are associated with depression.
Also, researchers have found that depression and anxiety often coexist; this explains how neurotransmitters influence each other.
John, a 34-year-old man, had been struggling with depression for years, feeling constantly drained, disconnected, and hopeless.
He described his depression as if his head were underwater, making it impossible for him to breathe, think, or see.
After trying therapy on his own with Cognitive Behavioral Therapy (CBT) but still feeling stuck, his psychologist suggested the use of antidepressant medication to restore the expected level of brain neurotransmitters, and John accepted.
This decision turned things around for him—within months, he began to feel a lot more like himself. He regained interest in things he loved, his energy returned, and life felt brighter again.
John’s story shows that even when things feel heavy, it’s possible to find the proper support and treatment that can help bring light back into your life. You’re not alone, and there’s always hope for better days ahead.
This journey underscores an important reality: depression is complex, with various contributing factors ranging from neurotransmitter imbalances to psychological stress, genetics, and life events.
Understanding how these elements interconnect and impact our brain and body is crucial in recognizing the importance of early intervention and treatment.
Whether through therapy, medication, or lifestyle changes, addressing depression effectively involves a comprehensive approach tailored to individual needs.
So, if you’re struggling, know that seeking help is the first step toward regaining balance and hope. The path to recovery is possible, and with the proper support, brighter days await.

References
- Centers for Disease Control and Prevention. (n.d.). Facts about suicide. https://www.cdc.gov/suicide/facts/index.html
- Hedegaard, H., Curtin, S. C., & Warner, M. (2021). Suicide mortality in the United States, 1999–2019 (NCHS Data Brief No. 213). National Center for Health Statistics. https://www.cdc.gov/nchs/data/nhsr/nhsr213.pdf
- American Psychiatric Association. (n.d.). DSM-5-TR fact sheets. https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/dsm-5-tr-fact-sheets
- National Institute for Health and Care Excellence. (2019). Preventing suicide: A technical package of policy, programs, and practices. https://www.ncbi.nlm.nih.gov/books/NBK538248/
- Harvard Health Publishing. (n.d.). The dopamine connection. Harvard Medical School. https://www.health.harvard.edu/mind-and-mood/the_dopamine_connection
- Mayo Clinic Staff. (2019). Antidepressants: Selecting one that’s right for you. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20046273
- National Center for Biotechnology Information. (n.d.). Bullying and suicide: What we know and what it means for schools. https://www.ncbi.nlm.nih.gov/books/NBK526124/
- Kondo, K., et al. (2022). Suicide prevention interventions and their effectiveness: A systematic review. BMC Psychiatry, 22, Article 470. https://pmc.ncbi.nlm.nih.gov/articles/PMC9180936/
- Wittchen, H. U., et al. (2011). The burden of mood disorders. European Neuropsychopharmacology, 21(9), 655–679. https://pmc.ncbi.nlm.nih.gov/articles/PMC4957550/
- Kessler, R. C., et al. (2000). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives of General Psychiatry, 57(8), 617–627. https://pubmed.ncbi.nlm.nih.gov/10964842/
- Moussavi, S., et al. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet, 370(9590), 851–858. https://pubmed.ncbi.nlm.nih.gov/20187598/
- Lépine, J. P., & Briley, M. (2011). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3–7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5562427/
- Sadock, B. J., et al. (2012). Comorbidity in mental illness. Comprehensive Psychiatry, 53(1), 1–5. https://pubmed.ncbi.nlm.nih.gov/23072492/
- Smith, J. (2012). The influence of stress on mental disorders. Health, 4(9), 597–602. https://www.scirp.org/reference/referencespapers?referenceid=796987
- Kessler, R. C., et al. (2012). The epidemiology of major depressive disorder. Psychological Medicine, 42(6), 1229–1239. https://pubmed.ncbi.nlm.nih.gov/22867077/
- Sherin, J. E., & Nemeroff, C. B. (2011). Post-traumatic stress disorder: The neurobiological impact of psychological trauma. Dialogues in Clinical Neuroscience, 13(3), 263–278. https://pmc.ncbi.nlm.nih.gov/articles/PMC3182008/
- Shapero, B. G., et al. (2014). Stressful life events and depression symptoms: The effect of childhood emotional abuse on stress reactivity. Journal of Clinical Psychology, 70(3), 209–223. https://pmc.ncbi.nlm.nih.gov/articles/PMC3884028/
- Kendler, K. S., et al. (1999). Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry, 156(6), 837–841. https://psycnet.apa.org/record/2008-07755-000
- Felitti, V. J., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. https://www.ajpmonline.org/article/S0749-3797%2898%2900017-8/fulltext
- Pine, D. S., et al. (2000). Childhood anxiety and depression: A review of the literature. Child and Adolescent Psychiatric Clinics, 9(1), 1–19. https://pubmed.ncbi.nlm.nih.gov/15289279/
- Naicker, K., et al. (2017). Type 2 diabetes and comorbid symptoms of depression and anxiety: Longitudinal associations with mortality risk. Diabetes Care, 40(3), 352–358. https://diabetesjournals.org/care/article/40/3/352/36943/Type-2-Diabetes-and-Comorbid-Symptoms-of
Inoue, K., et al. (2020). Depression and cardiovascular disease events among patients with type 2 diabetes: A systematic review and meta-analysis. Journal of Diabetes and Its Complications, 34(12), 107710. https://pmc.ncbi.nlm.nih.gov/articles/PMC7467011/
