Understanding Sickle Cell Disease in BIPOC Communities

About 20 million people worldwide and 100,000 in the USA are diagnosed with sickle cell disease, with most of them being part of the BIPOC community. Indeed, 1 in 13 Black babies is born with the sickle cell trait (Sickle Cell Disease – What Is Sickle Cell Disease?, 2024).
This statistic necessitates increasing awareness regarding sickle cell disease (SCD), an inherited red blood disorder (a disruption of normal body function) that usually results in anemia (a decreased red blood cell count) and may progress to sickle cell crisis (episodes of extreme pain).
This blog aims to highlight the challenges and increase awareness within the BIPOC community regarding sickle cell disease, its symptoms, treatment, and why it is most common among African Americans.
What is sickle cell

Understanding the mechanism of sickle cell disease will help us understand the disease. The main problem is a genetic mutation in red blood cells that results in the abnormal shape of hemoglobin, a component that carries oxygen to the rest of the body.
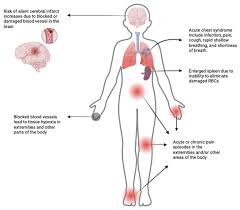
Subsequently, abnormal red blood cell shape, this new “sickle-shaped” shape, results in many problems, such as blockage of the bloodstream as the cells accumulate due to their shape, causing Vascular Occlusion (blockage), then painful crises.
Thus, blockage of blood flow is the worst complication, as it leads to a decrease in oxygen delivery, resulting in stroke and organ failure. In these conditions, the patients require hospitalization for artificial oxygen and blood supply.
Blood supply is needed because sickle-shaped cells have a short lifespan. They tend to undergo hemolysis, breaking down red blood cells (RBC).
This results in a decrease in the number of red blood cells and the release of hemoglobin in the bloodstream, known as anemia.
Then, the patient’s immune system becomes weak to fight against infection; even a common cold could make him sick. In addition, body organs, including the spleen, liver, kidneys, and lungs, start to collapse.
Why It Primarily Affects BIPOC Communities
Sickle cell disease (SCD) is the most common genetically inherited disease affecting African Americans (Sickle Cell Disease, n.d.).
The causes are unclear, but researchers suggest malaria as the predisposing factor. Malaria is a common disease in Africa due to the prevalence of mosquitoes in waterproofing. The body makes gene mutations to protect against malaria, and the gene is inherited to the existing generation.
Individuals carrying one copy of the mutated gene (sickle cell trait) have shown increased resistance to severe malaria infections. But, this protective mechanism leads to a higher prevalence of sickle cell traits in these areas.
It’s disheartening to learn that research conducted in 2022 revealed the heavy burden of malaria in Africa. The results showed that the African region bore 94% of cases and 95% of deaths globally, with 233 million malaria cases and 580000 deaths. It’s saddening that there was only a slight reduction compared to 2021(Malaria | Who | Regional Office for Africa, 2025).
The cause of sickle cell
The cause is a genetic mutation, which means a change in the DNA component through swapping, adding, or deleting.
In our case, it is a point mutation in the hemoglobin gene known as HBB. This mutation produces abnormal hemoglobin called hemoglobin S (HbS)(Kavanagh et al., 2022).
Hemoglobin is a protein in red blood cells that carries oxygen from the lungs to the rest of the body and returns carbon dioxide to the lungs to exhale. A change in the structure of hemoglobin causes the red blood cells to become unable to carry oxygen(Hbb Gene, 2024).
As a result, the mutation makes red blood cells, instead of round and flexible, become stiff and crescent-shaped (like a sickle), which causes various health complications, including pain, anemia, and organ damage.
Remember, sickle cell disease is an autosomal inherited disease, which means the patient must have both genes from his parents to confirm the diagnosis; otherwise, you will be a disease carrier.
You may be a disease carrier in malaria unless both parents have the muted gene. Then, you are at risk of developing sickle cell disease(“Inheritance of Sickle Cell Anaemia » Sickle Cell Society,” n.d.).
Symptoms and Complications of Sickle Cell Disease
Symptoms can differ significantly from person to person, as sickle cell disease is a disorder that impacts various organs based on their ability to defend against illness. Below are the most common signs and symptoms, along with their potential complications:
1. Anemia:
As a result of hemolysis and decreased red blood count, anemia develops and leads to:
- Fatigue: A feeling of extreme tiredness, exhaustion, or lack of energy
- Weakness: A lack of physical strength or muscle power
- Shortness of breath: When oxygen levels are low, your body tries to compensate by breathing faster, making you feel out of breath even with little activity.
- Dizziness: The brain needs oxygen to function correctly. Anemia reduces oxygen flow, leading to lightheadedness, dizziness, or fainting.
Anemia makes your heart work harder to provide oxygen to the body; this extra work can strain your heart and lead to complications like heart murmurs, cardiac hypertrophy (an increase in the size of the heart’s muscle), and heart failure.
Finally, it may lead to collapse, which is a multiple organ failure that could lead to death (Are All Heart Murmurs Serious?, n.d.).
2.Jaundice:
A condition of yellow skin and eyes caused by an excess of bilirubin in blood, a yellow pigment released by faster hemolysis of red blood cells.
It appears as:
- Yellowing of the skin and eyes
- Dark-colored urine
- Pale stools
- Itching
3. Episodic pain (pain crisis):
Red blood cells usually move from the heart to organs. When sickle cells move, they get stuck and prevent blood flow, which leads to severe pain that usually occurs suddenly in the chest, legs, and arms.
4. Acute chest syndrome:
A sudden blockage of the lung’s blood vessels could be life-threatening, as it decreases oxygen delivery to the brain. Symptoms of this condition include fever, pain, and cough.
5. Swelling in Hands & Feet:
Block of blood vessels results in accumulation of blood, which could be a source of infection.
6. Frequent Infections:
The spleen plays a significant role in defense against infection; if it is damaged, people may be vulnerable to infections.
Treatment and Advances in Sickle Cell Care
1. Medications:
The U.S. Food and Drug Administration (FDA) has approved the following drugs to treat sickle cell disease.
- Hydroxyurea
- L-glutamine
- Crizanlizumab-tmca
Both drugs prevent the sickling of red blood cells through different mechanisms. As a result, symptoms are decreased and complications are reduced. However, the drugs are unable to cure sickle cell disease.
They also approve the use of some drugs like acetaminophen or ibuprofen for mild to moderate pain. In case of severe pain, the doctor may prescribe opioids a specific pain medications(Sickle Cell Disease – Treatment | Nhlbi, Nih, 2024).
2. Bone marrow transplant:
Bone marrow transplants successfully cure sickle cell disease, particularly in 90% of children and adolescents, yet transplant is risky in adults, but Scientists are studying new ways for transplant.
It mainly works by replacing the affected bone marrow that produces red blood cells with normal bone marrow from matched donors, usually siblings(Sickle Cell Disease – Treatment | Nhlbi, Nih, 2024).
However, it’s important to note that bone marrow transplant carries risks in addition to complications from the transplant process.
St. Jude Children’s Research Hospital revealed that patients not only experienced a cure for sickle cell disease but also showed improvement in affected organs such as the heart(Bone Marrow Transplantation for Sickle Cell Disease Improves Myocardial Fibrosis, n.d.).
Gene Therapy: A New Hope for Sickle Cell Patients:
It is the process of adding or changing DNA. There are two gene therapy methods to cure sickle cell disease.
1. Exagamglogene autotemcel: Insert a modified gene into the body.
2. Lovotibeglogene autotemcel:Change the existing gene.
These two methods modify the stem cell, which is responsible for producing red blood cells; they could be helpful for people who don’t have a matched donor.
Sickle cell disease remains challenging for the PIBOC community due to genetic inheritance; therefore, being aware of the disease, its causes, symptoms, and possible complications is essential for better management and reducing its impact.
The good news is gene therapy and bone marrow transplants provide hope for the future despite complications, but Scientists are still working on improvement.
